I wish someone, besides my doctor, had told me that pregnancy was not a license to lose control over my eating habits. Here’s what I learnt about the risk between obesity and Gestational Diabetes while pregnant.
Today, I’m talking about Gestational Diabetes, but let me start by sharing an encounter.
Doctor: Mrs. Bolaji-Olojo, I am going to send you off for a blood sugar test. Please bring the result to your next appointment, next week.
Me: Excuse me sir! Next week what? This baby is coming out this week, and I will have no need to see you with any blood sugar test result next week.
Okay, to be honest, my response wasn’t that confident, but I made it clear to the doctor—who I was seeing for the first time on antenatal— that I wouldn’t be doing the test, and I that I wouldn’t need the antenatal the next week because my baby was just about ready to pop. I was 37 weeks gone, and about 106 kg at the time, so really, I was tired of being pregnant. I was also so sure my baby wouldn’t hit the 38 week mark. However, I was concerned as to why the doctor would ask me to do a blood sugar test. Since I decided not to do it, I did not bother to ask him why. But my best friend, also a Medical Doctor, asked me what I weighed at the time. When I told her, she said that was why the doctor had sent me off for the blood sugar test. Usually, when a woman’s weight increases so much during pregnancy, especially to over a 100 kg, the doctors want to rule out the possibility of Gestational Diabetes. GD sometimes presents no signs or symptoms, but if left unchecked can affect both the mother and the baby.
What is Gestational Diabetes (GD)?
Like other forms of diabetes, Gestational Diabetes affects how the body uses and breaks down sugar/glucose. The difference is that this form of diabetes occurs only in pregnant women, including but not limited to those who were not diabetic before pregnancy. For many women, it develops in later stages of pregnancy and can lead to labour complications if not controlled. Other implications include having a macrosomic baby, which is a baby with a birth weight of more than 4kg (8lbs 8oz), as well as the increased risk of Type 2 Diabetes for the mother after pregnancy.
Causes of Gestational Diabetes (GD)
A family history of diabetes, diabetes diagnosed just before pregnancy, or Gestational Diabetes in a previous pregnancy are all risk factors for a number of women. However, the most recurring factor is OBESITY; that is a high amount of body fat and weight gain, especially during pregnancy. The good thing is, while we may have no control over the earlier risk factors stated, we certainly have control over obesity, by controlling our lifestyle while pregnant.
In my opinion, pregnancy is such a beautiful and sensitive season in a woman’s life. She is responsible for a whole and totally dependent human being, so I believe the mother-to-be must make decisions that are not selfish. This is why I wonder how I thought it was okay to eat what I wanted, and in any portion I wanted just because I was pregnant. To make matters worse, society reinforces this belief by encouraging pregnant women to eat everything possible. I wish someone, besides my doctor, had told me that pregnancy was not a license to lose control over my eating habits. I would have really appreciated it. As a fellow woman, a good friend and a fitness coach, this is me telling you dear Preggo, that Gestational diabetes is real, and because I know you love yourself and your baby, you would want to be intentional about nourishing your body and providing the best environment for him/her to thrive.
Reducing the Risk

Carbs, a staple part of the Nigerian diet, are awesome and provide energy for the body, but they are also high in calories, and the body breaks them down and converts them to sugar. So our consumption of carbs while pregnant should be controlled. This is how it works in practical terms: Your body breaks down food, uses the energy it needs, burns more energy when you work out and then, stores the unused parts of the food as fat. This ultimately leads to a rise in the number on the scale. So the idea is to eat just what the body needs to function optimally, even when you are pregnant, to reduce the chances of storing the excess as fat. This is why your body weight is monitored at every antenatal visit, to make sure you are gaining weight slowly as your pregnancy progresses, totaling an average of 12 to 15 kg for a normal and single fetus pregnancy.
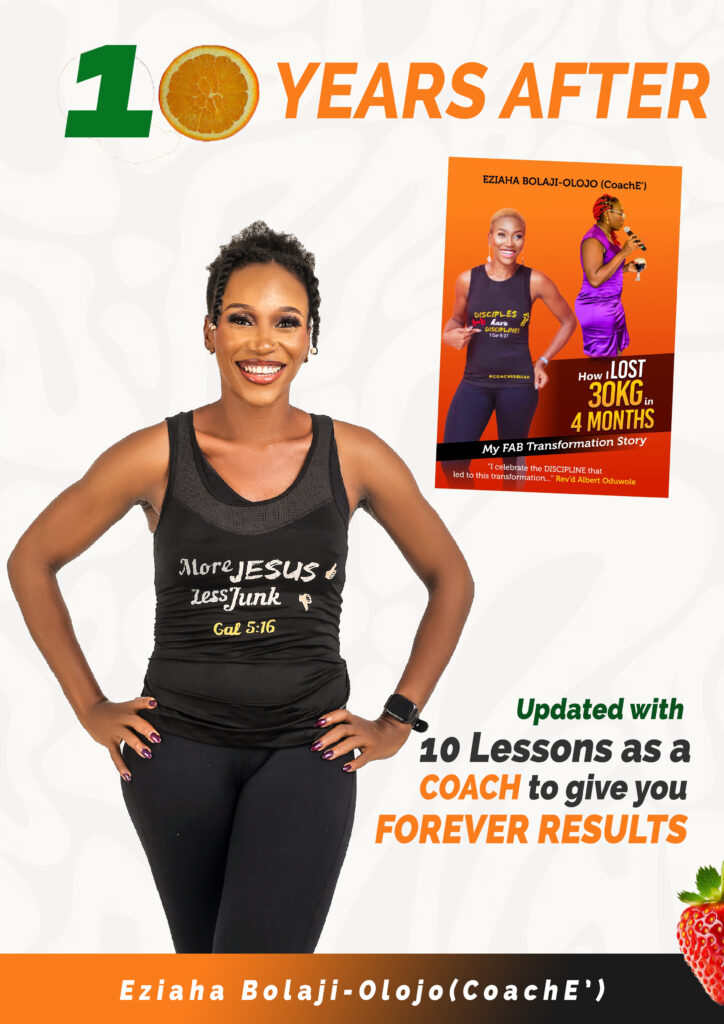
If Gestational Diabetes has already been diagnosed, the woman may need monitoring and medication to control it, but it can also and must be controlled with a healthy prenatal diet and exercise, where the woman is able to. This is not to say that carbs should be cut out of a pregnant woman’s diet, but that a good GD diet, created by a Professional, will control the quality and quantity of carbs to ensure that the woman still has enough energy while controlling the blood sugar. As for me, I eventually saw that doctor again, and again, and again, because I was eventually induced at 42 weeks, after hitting 111 kg. Although my test results (yes, I finally did the test) didn’t indicate the presence of GD, I did have a traumatic labour experience, and a macrosomic baby (4.4kg) who needed blood sugar monitoring at NICU for a couple of days. Thankfully, we both made it, but it taught me a lesson, so I made up my mind that the next pregnancy would be a different experience. And it totally was.

And now I help more preggos rock their bump with some discipline. 09055868614 is our coaching line


Oh thank you for this post once again.am to do my test in about 2 weeks and I hve been frantic
I have started making changes to my diet eating more vegetables God bless you.
Read this again in preparation for baby number two. I am gathering all the useful information in advance. Looking forward to nurturing another life in this body. This time, better.
That’s the spirit?. Thanks for reading A